Recently we learn that Yoga can treat depression.

This new researches give more thumbs up to yoga. You can also fight your back pain without medicine which you can check in my other blog.

How Does Yoga Work to reduce back pain?

Yoga helps you physically by making your muscles, tissues and joints healthy and also improves the function of your organs, immune system and glandular system, e.g. your digestion, breathing, gynaecological health and nervous system can improve too. Yoga is a mind/body discipline, positively affecting your body and mental outlook. Research shows that people with low back pain are less depressed after 3 months of being offered yoga and also after practising yoga at home a year after beginning. Our trial backs up two past trials (K. Williams et al 2009 and E. Groessl et al 2008) in suggesting that depression in low back pain sufferers decreases with yoga and that yoga’s benefits are long-term. It can be depressing to have back pain and yoga helps to bring about positive mental changes.
Research shows that the Alexander Technique (postural awareness), Cognitive Behavioural Therapy, manipulation and exercise can help to reduce back pain. Yoga can combine similar elements from all these methods into a single treatment package. You learn to use your body efficiently and comfortably throughout your day by attention to your postural habits – which is very relevant to recurrent back pain. You learn to change your attitude to your back pain episodes and also to the experience of occasional pain itself with self-observation and by targeting the neurological pathways from the site of pain to the brain. You learn to gently bring mobility to stiff parts of your body and to keep them flexible. which encourages future health in those areas. You learn to exercise, strengthen and relax your body and also your mind, with beneficial effects to your body, your mind and your whole being.

Why back pain?
Experts say that back pain is associated with the way our bones, muscles and ligaments in our backs work together. Pain in the lower back may be linked to the bony lumbar spine, discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, lower back muscles, abdomen and pelvic internal organs, and the skin around the lumbar area. Pain in the upper back may be due to disorders of the aorta, tumors in the chest, and spine inflammation.
What are the causes of back pain?
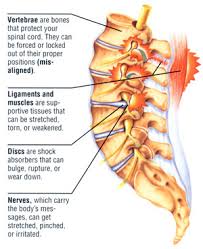
The human back is composed of a complex structure of muscles, ligaments, tendons, disks and bones - the segments of our spine are cushioned with cartilage-like pads. Problems with any of these components can lead to back pain. In some cases of back pain, its cause is never found.
Strain - the most common causes of back pain are:
Strained muscles
Strained ligaments
Lifting something improperly
Lifting something that is too heavy
The result of an abrupt and awkward movement
A muscle spasm
Structural problems - the following structural problems may also result in back pain:
Ruptured disks - each vertebra in our spine is cushioned by disks. If the disk ruptures there will be more pressure on a nerve, resulting in back pain.
Bulging disks - in much the same way as ruptured disks, a bulging disk can result in more pressure on a nerve.
Sciatica - a sharp and shooting pain that travels through the buttock and down the back of the leg, caused by a bulging or herniated disk pressing on a nerve.
Arthritis - patients with osteoarthritis commonly experience problems with the joints in the hips, lower back, knees and hands. In some cases spinal stenosis can develop - the space around the spinal cord narrows.
Abnormal curvature of the spine - if the spine curves in an unusual way the patient is more likely to experience back pain. An example is scoliosis, when the spine curves to the side.
Osteoporosis - bones, including the vertebrae of the spine, become brittle and porous, making compression fractures more likely.
Cauda equina syndrome - the cauda equine is a bundle of spinal nerve roots that arise from the lower end of the spinal cord. People with cauda equine syndrome feel a dull pain in the lower back and upper buttocks, as well as analgesia (lack of feeling) in the buttocks, genitalia and thigh. There are sometimes bowel and bladder function disturbances.
Cancer of the spine - a tumor located on the spine may press against a nerve, resulting in back pain.
Infection of the spine - if the patient has an elevated body temperature (fever) as well as a tender warm area on the back, it could be caused by an infection of the spine.
Other infections - pelvic inflammatory disease (females), bladder or kidney infections.
Sleep disorders - individuals with sleep disorders are more likely to experience back pain, compared to others.
Shingles - an infection that can affect the nerves.
Bad mattress - if a mattress does not support specific parts of the body and keep the spine straight, there is a greater risk of developing back pain.

Diagnosing back pain
Most GPs (general practitioners, primary care physicians) will be able to diagnose back pain after carrying out a physical examination, and interviewing the patient. In the majority of cases imaging scans are not required.
If the doctor and/or patient suspect some injury to the back, tests may be ordered. Also, if the doctor suspects the back pain might be due to an underlying cause, or if the pain persists for too long, further tests may be recommended.
Suspected disc, nerve, tendon, and other problems - X-rays or some other imaging scan, such as a CT (computerized tomography) or MRI (magnetic resonance imaging) scan may be used to get a better view of the state of the soft tissues in the patient's back.
X-rays can show the alignment of the bones and whether the patient has arthritis or broken bones. They are not ideal for detecting problems with muscles, the spinal cord, nerves or disks.
MRI or CT scans - these are good for revealing herniated disks or problems with tissue, tendons, nerves, ligaments, blood vessels, muscles and bones.
Bone scan - a bone scan may be used for detecting bone tumors or compression fractures caused by brittle bones (osteoporosis). The patient receives an injection of a tracer (a radioactive substance) into a vein. The tracer collects in the bones and helps the doctor detect bone problems with the aid of a special camera.
Electromyography or EMG - the electrical impulses produced by nerves in response to muscles is measured. This study can confirm nerve compression which may occur with a herniated disk or spinal stenosis (narrowing of the spinal canal).
What are the treatment options for back pain?
In the vast majority of cases back pain resolves itself without medical help - just with careful attention and home treatment. Pain can usually be addressed with OTC (over-the-counter, no prescription required) painkillers. Resting is helpful, but should not usually last more than a couple of days - too much rest may actually be counterproductive.
Usually back pain is categorized into two types:
Acute - back pain comes on suddenly and persists for a maximum of three months.
Chronic - the pain gradually develops over a longer period, lasts for over three months, and causes long-term problems.
A considerable percentage of patients with back pain experience both occasional bouts of more intense pain as well as more-or-less continuous mild back pain, making it harder for the doctor to determine whether they have acute or chronic back pain.
If home treatments do not give the desired results, a doctor may recommend the following:
Medication - back pain that does not respond well to OTC painkillers may require a prescription NSAID (nonsteroidal anti-inflammatory drug). Codeine or hydrocodone - narcotics - may also be prescribed for short periods; they require close monitoring by the doctor.
Some tricyclic antidepressants, such as amitriptyline, have been shown to alleviate the symptoms of back pain, regardless of whether or not the patient has depression.
Physical Therapy - the application of heat, ice, ultrasound and electrical stimulation, as well as some muscle-release techniques to the back muscles and soft tissues may help alleviate pain. As the pain subsides the physical therapist may introduce some flexibility and strength exercises for the back and abdominal muscles. Techniques on improving posture may also help. The patient will be encouraged to practice the techniques regularly, even after the pain has gone, to prevent back pain recurrence.
Cortisone injections - if the above-mentioned therapies are not effective enough, or if the pain reaches down to the patient's legs, cortisone may be injected into the epidural space (space around the spinal cord). Cortisone is an anti-inflammatory drug; it helps reduce inflammation around the nerve roots. According to The Mayo Clinic, USA, the pain-relief effect will wear off after less than six weeks.
New Research-Yoga Could Be a Cost-effective Treatment For Back Pain

According to research published in Spine, the yoga intervention program called 'Yoga for Healthy Lower Backs' is most likely going to be cost effective for not only the UK National Health Service (NHS), but for the wider society as well.

The specially-developed 12-week group yoga intervention program was observed and compared to conventional general practitioner (GP) care alone.

In order to decide if this was an appropriate use of NHS resources, the cost of the program needed to be checked out. There are currently no available yoga classes through the NHS which is why the team wanted to find the likely cost of a program. After much examination, the experts, from the University of York's Department of Health Sciences and the Centre for Health Economics, and the Hull York Medical School, concluded that there was a high chance (around 70%) of the yoga intervention being cost effective if the cost remained below £300 per patient (for a cycle of 12 classes).Results also showed that

participants in the control group had more days off work than those in the yoga program. After reporting back pain, a control group participant took an average of 12 days off. The cost associated with this control group participant's time off was £1,202, as opposed to £374 for a yoga group member. Professor David Torgerson, lead author and Director of York Trials Unit, in the University of York's Department of Health Sciences, said: "Back pain represents a significant burden to the NHS in the UK and to society as a whole. As well as the associated health care costs, it is also a major cause of work absenteeism which leads to a productivity loss to society.

participants in the control group had more days off work than those in the yoga program. After reporting back pain, a control group participant took an average of 12 days off. The cost associated with this control group participant's time off was £1,202, as opposed to £374 for a yoga group member. Professor David Torgerson, lead author and Director of York Trials Unit, in the University of York's Department of Health Sciences, said: "Back pain represents a significant burden to the NHS in the UK and to society as a whole. As well as the associated health care costs, it is also a major cause of work absenteeism which leads to a productivity loss to society.
He continued to explain how there has been little research on yoga's cost effectiveness, even though evidence has shown the benefits for people with chronic and low back pain. "In our study we evaluated a specially-designed yoga class package by using individual-level data from a multi-centred randomized controlled trial. On the basis of the 12-month trial, we conclude that 12 weekly group classes of specialised yoga are likely to provide a cost-effective intervention for the treatment of patients with chronic or recurrent low back pain. Back pain is one of the most common medical conditions treated in primary care in the U.K., costing the NHS about £1.37 billion and the health care sector £2.10 billion a year. Each year, an estimated 2.6 million people suffer with back problems and turn to their GP for advice.
Professor Alan Silman, Medical Director of Arthritis Research UK, said, We welcome the fact that not only has yoga been found to help people manage their back pain, but that it is also cost effective, and results in fewer sick days. It is another option for people who are struggling to manage their condition, and one that encourages the move to self-management. Yoga is an intervention that has been proven to make their everyday lives easier and their pain more manageable. We'd hope that on the back of this, more people with back pain are encouraged to take up the yoga program.
Participants who had either chronic or recurrent back pain were examined in the trial, who were split up into one group of 156 people offered yoga classes designed to improve their back, and a second control group of 157 who received GP care alone. Each group had regular GP care, either involving medication to relieve pain or a referral to pain clinics and physiotherapists.
The program was designed to last for 12-weeks by Alison Trewhela, an Iyengar Yoga teacher and Senior Practitioner in Yoga on the British Register of Complementary Practitioners, with yoga teacher Anna Semlyen, a Back Care Advisor to the British Wheel of Yoga. Twelve professional yoga teachers delivered the work out. Alison Trewhela concluded, GPs and commissioners are showing great interest in this yoga program. Many consider it could be the primary treatment option because it offers long-term positive outcomes, as well as a multi-disciplinary combination of taught skills that suits the bio-psycho-social nature of the condition of chronic low back pain. Within its confidence-boosting, gradually-progressing environment, the gentle 'Yoga for Healthy Lower Backs' course addresses joint mobility, muscle-strengthening, emphasis on the breath, mental attitude to pain and perspective on life lessons, postural awareness and low back education, relaxation techniques, and advice about other potentially health-giving techniques and benefits.
(Source- Spine)
No comments:
Post a Comment